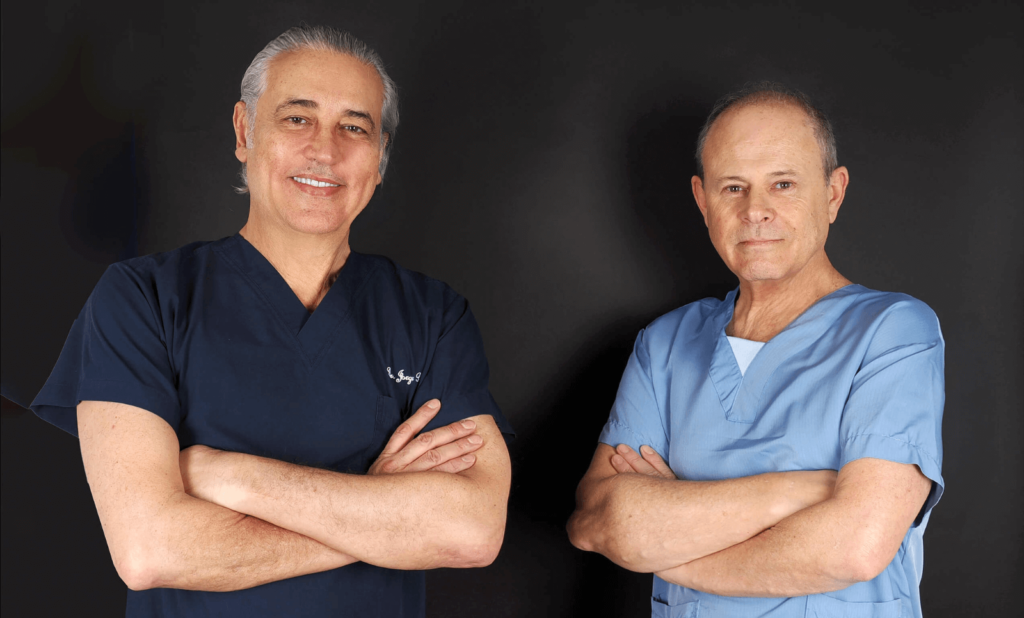
We are starting a series of conversations between Dr. Jorge Planas, plastic surgeon and medical director of Clínica Planas, and Dr. Miguel Garber, expert in regenerative medicine. We will explore how this innovative discipline is revolutionizing traditional medicine by enhancing the body’s natural repair processes, improving quality of life, and opening new therapeutic and aesthetic possibilities.
DR. JORGE PLANAS:
What is regenerative medicine?
DR. MIGUEL GARBER:
Regenerative medicine is a branch of modern medicine that aims to restore, repair, or replace cells, tissues, or organs that have been damaged by aging, diseases, or injuries.
Unlike traditional medicine, which often focuses on alleviating symptoms, regenerative medicine seeks to address the root cause of the problem by stimulating the body’s natural healing and repair mechanisms.
DR. JORGE PLANAS:
When we talk about “regenerating tissue,” what exactly are we referring to?
DR. MIGUEL GARBER:
When we say regenerating tissue, we are referring to restoring its original biological functions through various mechanisms:
- Reducing or preventing the formation of scars (fibrosis), which limit the tissue’s functionality.
- Improving vascularization, meaning promoting the formation of new blood vessels that ensure better delivery of oxygen and nutrients.
- Stimulating the recovery and proper functioning of the cells that make up the tissue.
- Eliminating so-called senescent cells, also known as “zombie cells,” which are aged cells that no longer perform their function but remain in the body, causing inflammation and deterioration.
When we manage to intervene in these four aspects, we can truly talk about regenerating a tissue or organ.
DR. JORGE PLANAS:
Are the lower back muscles, for example, considered a tissue?
DR. MIGUEL GARBER:
Exactly. The lower back area is made up of different tissues: bone, muscle, nerve, connective, and others. And all of them, to varying degrees, are susceptible to regeneration through regenerative therapies.
DR. JORGE PLANAS:
So, can the knee, lower back, hip, and cervical spine be regenerated?
DR. MIGUEL GARBER:
Yes, that’s right. Today, we have protocols that, by combining cells, growth factors, biomaterials, and other strategies, allow us to stimulate the regeneration of joint, bone, muscle, and tendon tissues, with the goal of restoring function and reducing chronic pain.
DR. JORGE PLANAS: Does regenerative medicine have scientific backing?
DR. MIGUEL GARBER:
While it still requires more scientific evidence, there are numerous clinical and preclinical studies that support its effectiveness. Regulatory bodies such as the FDA (U.S. Food and Drug Administration) and the EMA (European Medicines Agency) have approved various regenerative medicine therapies. Additionally, research in areas such as tissue engineering and cell therapy is advancing rapidly, with very promising results in the near future.
DR. JORGE PLANAS:
Is it true that regenerative medicine uses the body’s natural abilities to heal?
DR. MIGUEL GARBER:
Correct. The central approach is to enhance the mechanisms that the body already possesses for self-repair. Our role as doctors is to help restore that balance, creating the ideal conditions for the body to activate these mechanisms efficiently.
DR. JORGE PLANAS:
Could we then say that regenerative medicine “empowers” the body to heal itself?
DR. MIGUEL GARBER:
Exactly. The body always tries to repair itself, but sometimes, due to age, illness, or chronic stress, it loses that ability or does so incompletely. Regenerative medicine helps restore that potential.
DR. JORGE PLANAS:
Could you explain it with a more visual example?
DR. MIGUEL GARBER:
Sure. Let’s think of a cell as if it were a person:
- It needs food (nutrients).
- It needs oxygen.
- It needs a suitable environment to live in.
- And it must have energy to perform its function.
In regenerative medicine, we work on these four aspects:
- Nourishing the cell
- Oxygenating it
- Providing it with a healthy environment
- Stimulating its ability to produce energy.
Additionally, we can use therapies that “teach” the cell to behave in the right way, for example, activating anti-inflammatory, nutritional, and other processes.
DR. JORGE PLANAS:
So, just as joint tissues can be regenerated, can it also be done aesthetically, for example, on facial skin?
DR. MIGUEL GARBER:
Exactly. Tissue regeneration is not only applied in traumatology or degenerative diseases but also in aesthetic medicine. We can improve the quality and appearance of the skin through techniques that stimulate the production of collagen and elastin, restoring firmness and elasticity.
DR. JORGE PLANAS:
You mentioned the vascular stroma. What exactly is it?
DR. MIGUEL GARBER:
The vascular stroma is a fraction of adipose tissue (fat) that contains a diverse set of cells: mesenchymal stem cells, immune cells, pericytes, preadipocytes, endothelial cells, among others. This “cell cocktail” has a powerful regenerative effect, as it:
- Modulates inflammation
- Stimulates collagen production
- Promotes the formation of new blood vessels (neovascularization)
- Encourages cellular repair
DR. JORGE PLANAS:
So, for example, in a facial bio-stimulation treatment, are these cells from the vascular stroma used?
DR. MIGUEL GARBER:
Correct. In facial rejuvenation procedures, we extract a small amount of adipose tissue from the patient, process it to obtain the regenerative cells — mainly those from the vascular stroma — and reinject them into the areas to be treated.
These cells act in synergy with the environment, reducing inflammation, stimulating collagen and elastin production, and promoting skin regeneration from within.
DR. JORGE PLANAS:
And those circulating stem cells, when injected, do they work like that orchestra conductor you mentioned earlier?
DR. MIGUEL GARBER:
Exactly. These cells are smart: they adapt to the environment, and depending on what the tissue needs, they act accordingly. For example, if the skin needs to repair structural damage, the cells stimulate collagen production; if it needs to reduce inflammation, they release anti-inflammatory molecules; if the problem is vascular, they promote the formation of new capillaries.
We could say that they don’t always “play the same score.” They change their function according to the specific needs of the tissue, just like a conductor who adapts the music to each situation.