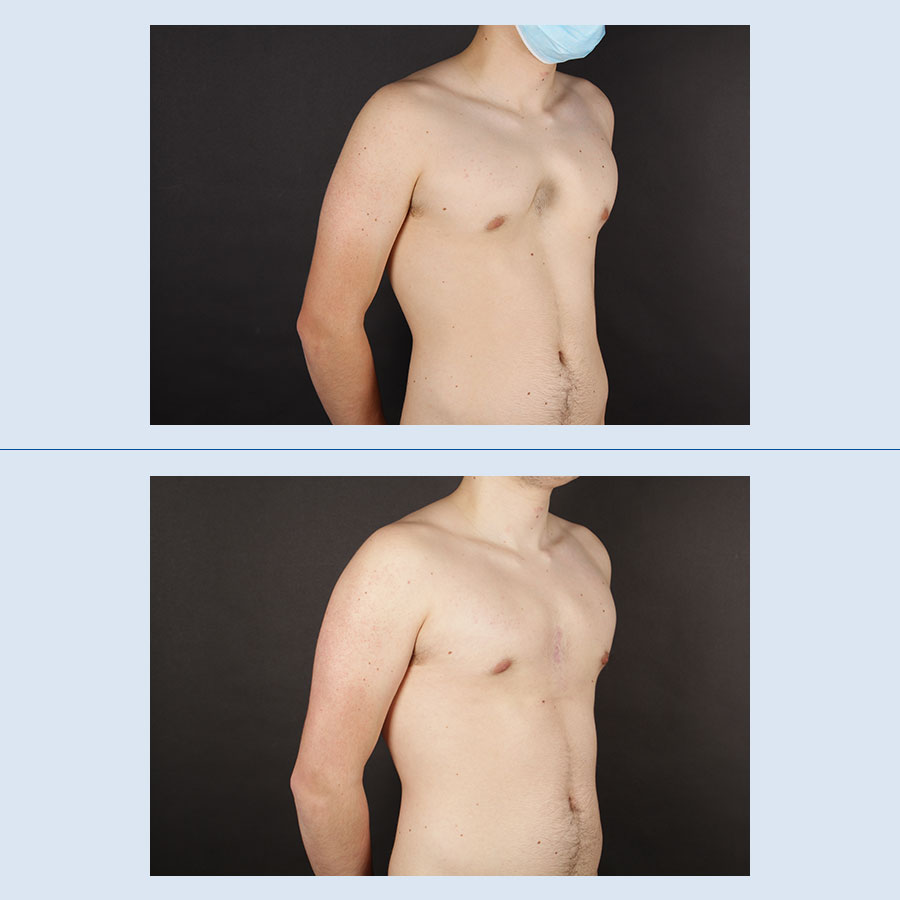
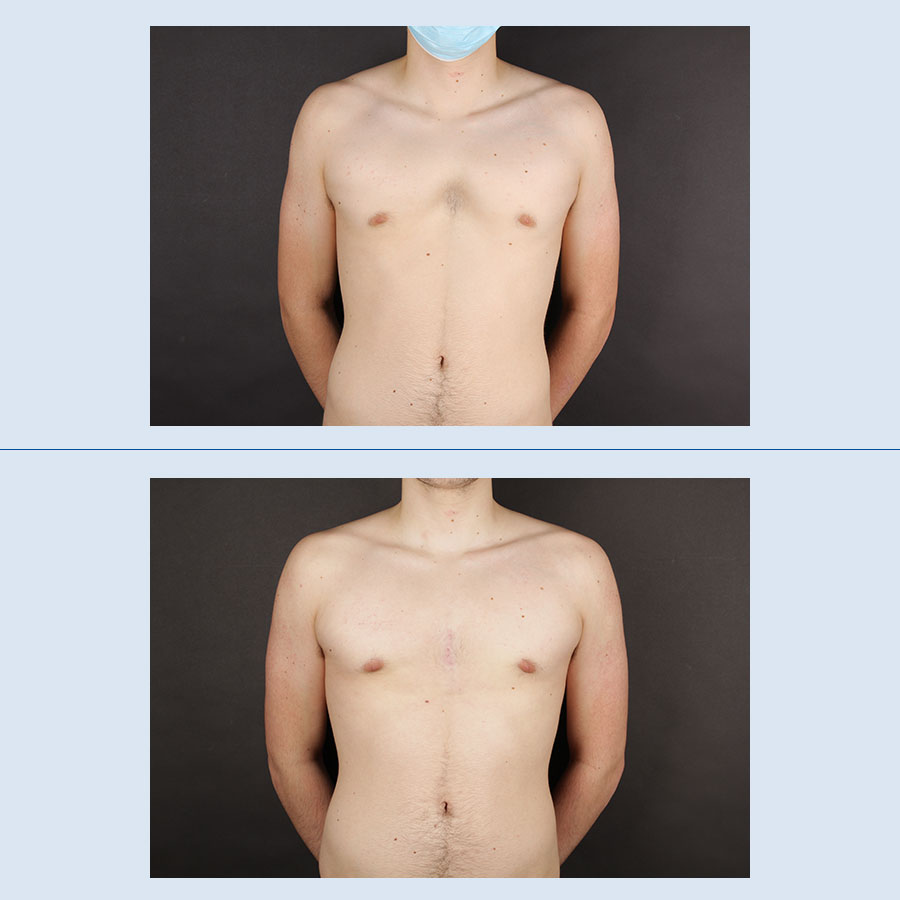
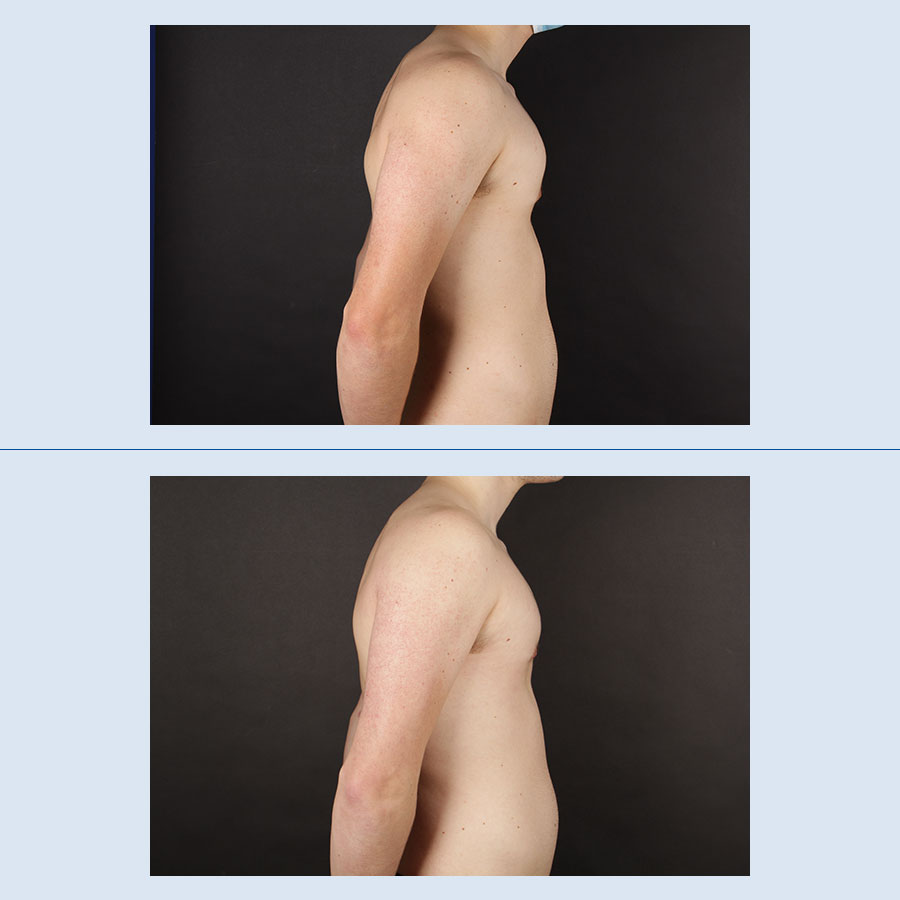
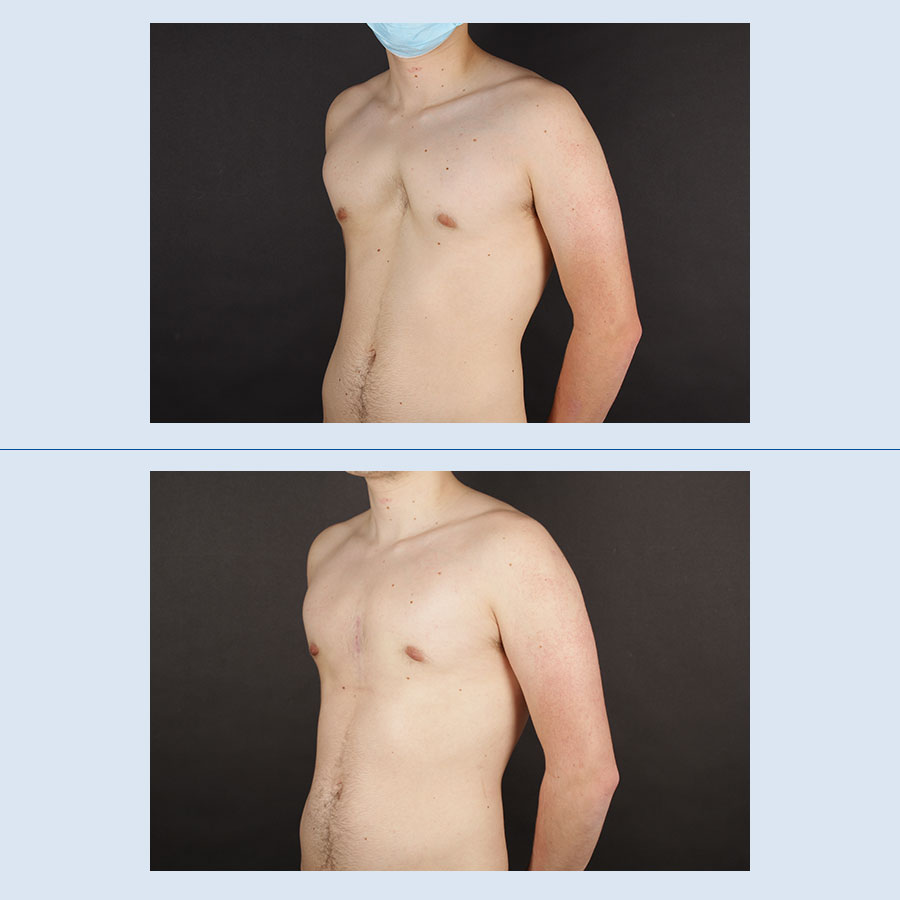
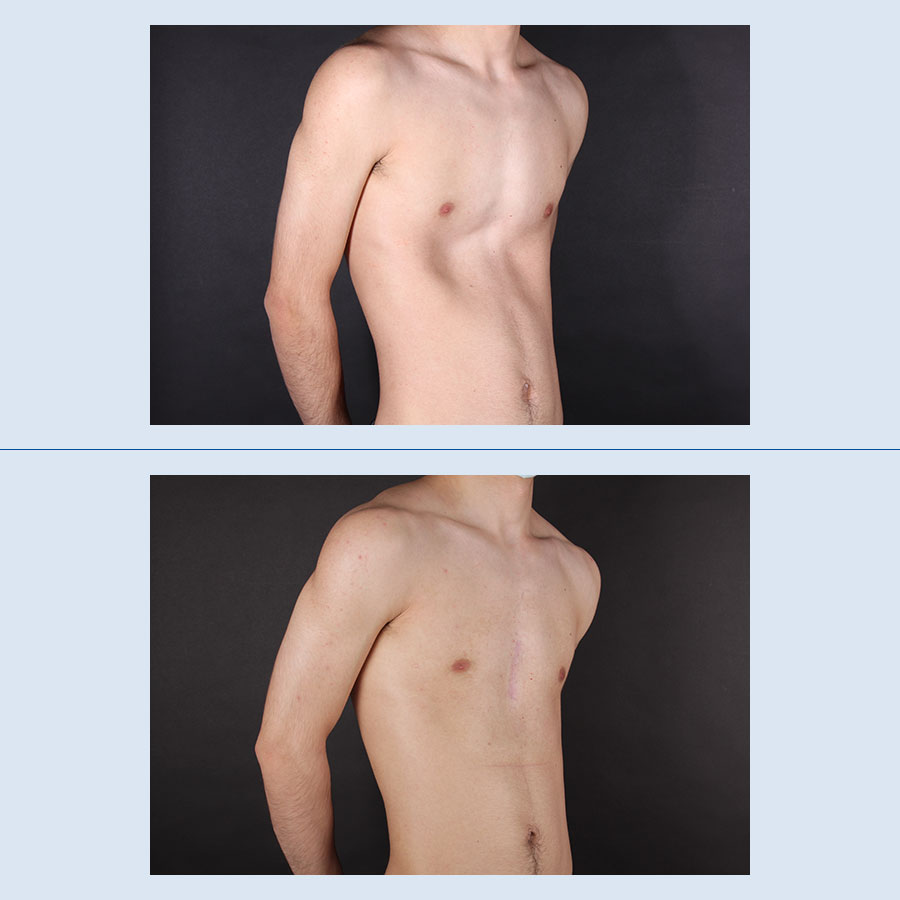
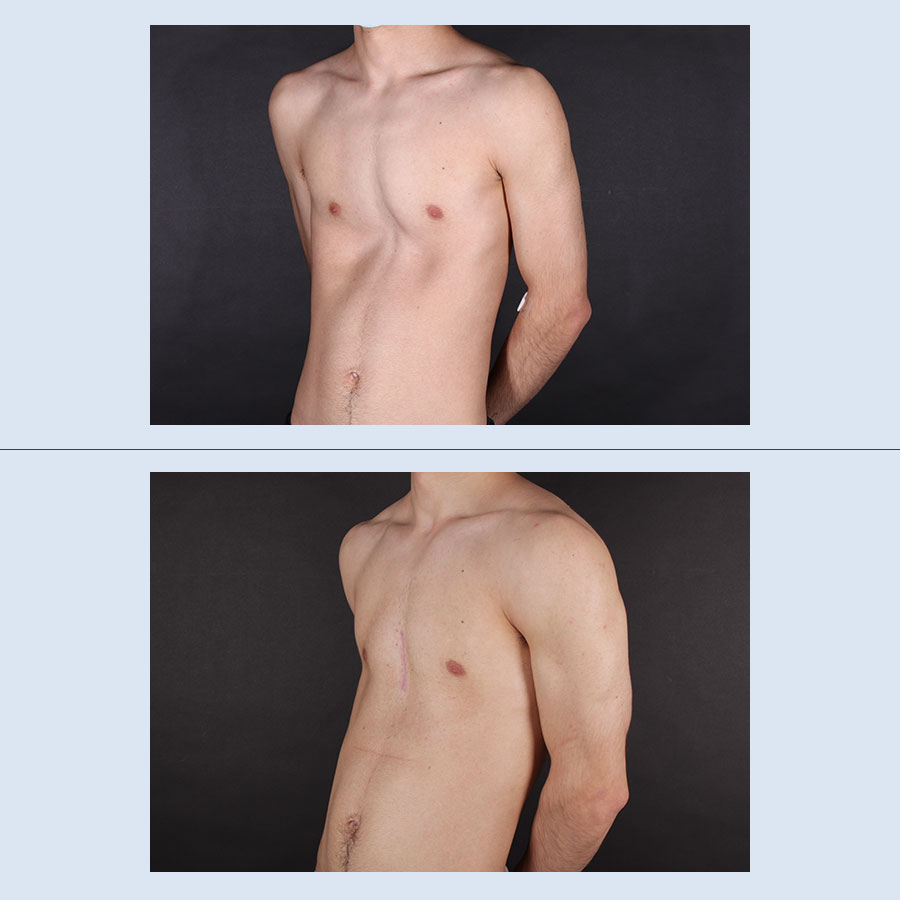
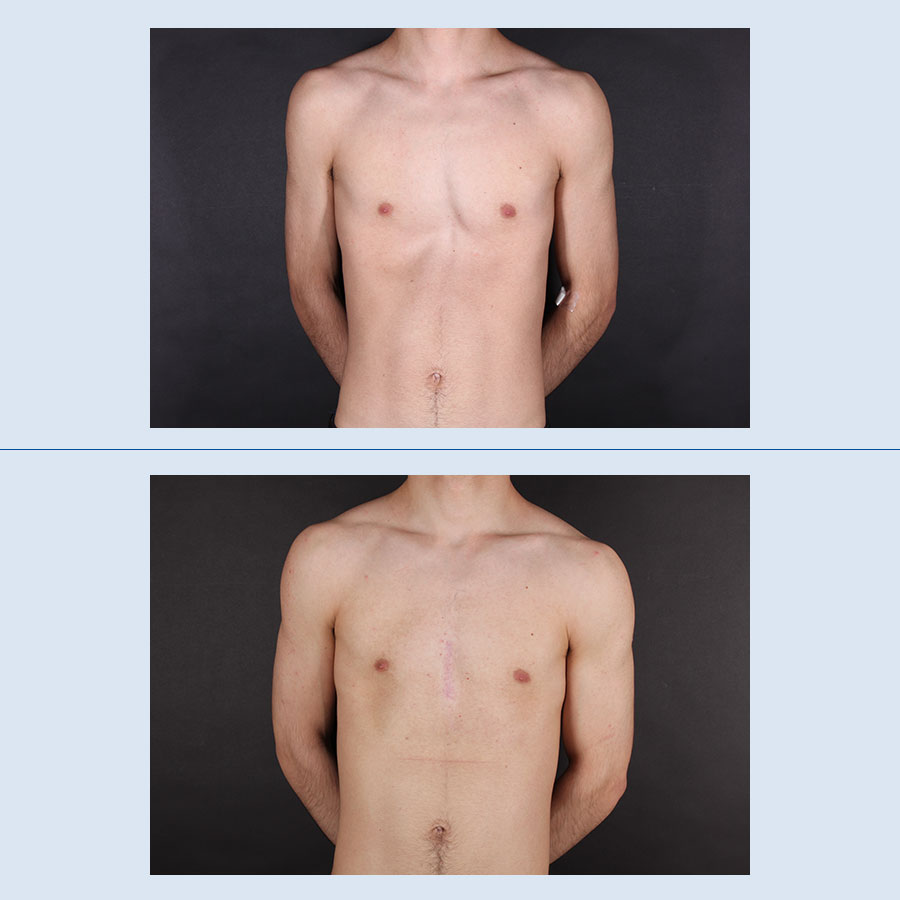
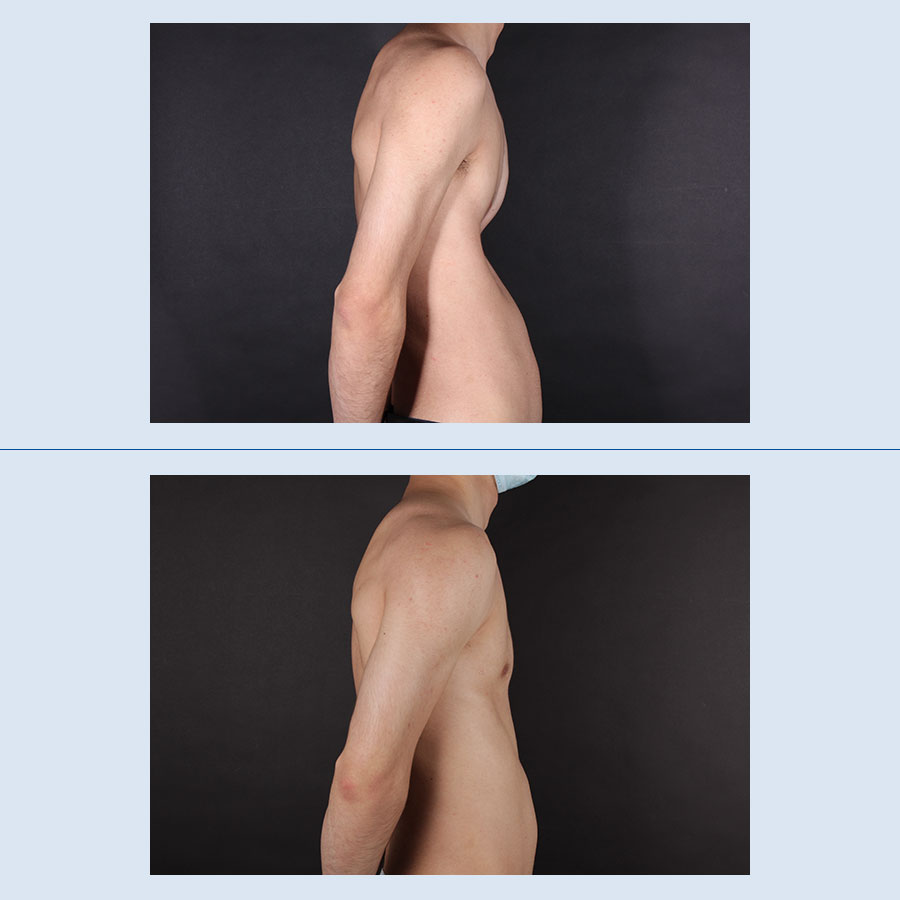
Pectus excavatum is a congenital deformity that often causes complexes and insecurities for those who suffer from it. Using a custom-made prosthesis created with 3D technology, we can effectively correct this deformity, with completely natural and permanent results.
Las cookies son pequeños archivos de datos que se reciben en el terminal desde el sitio Web visitado y se usan para registrar ciertas interacciones de la navegación en un sitio Web almacenando datos que podrán ser actualizados y recuperados. Estos archivos se almacenan en el ordenador del usuario y contiene datos anónimos que no son perjudiciales para su equipo. Se utilizan para recordar las preferencias del usuario, como el idioma seleccionado, datos de acceso o personalización de la página.
Las Cookies también pueden ser utilizadas para registrar información anónima acerca de cómo un visitante utiliza un sitio. Por ejemplo, desde qué página Web ha accedido, o si ha utilizado un "banner" publicitario para llegar.
¿Qué uso le damos a los diferentes tipos de cookies?Este sitio utiliza cookies técnicas, de personalización, análisis y publicitarias propias y de terceros, que tratan datos de conexión y/o del dispositivo, así como hábitos de navegación para fines estadísticos y publicitarios.
Por ello, al acceder a nuestra web, en cumplimiento del artículo 22 de la Ley de Servicios de la Sociedad de la Información le hemos solicitado su consentimiento para su uso.
El suministro de datos personales a través de nuestro portal y el consentimiento para el uso de cookies requiere una edad mínima de 14 años y la aceptación expresa de nuestra Política de Privacidad.
De todas formas, le informamos que puede activar o desactivar las cookies siguiendo las instrucciones de su navegador de Internet:
| Navegador | Pasos | URL |
|---|---|---|
| Chrome | Configuración > Mostrar opciones avanzadas > Privacidad > Configuración de contenido. | https://support.google.com/ |
| Firefox | Herramientas > Opciones > Privacidad > Historial > Configuración Personalizada | https://support.mozilla.org/ |
| Internet Explorer | Herramientas > Opciones de Internet > Privacidad > Configuración | https://support.microsoft.com/ |
| Opera | Herramientas > Preferencias > Editar preferencias > Cookies | https://help.opera.com/ |
| Safari | Preferencias > Seguridad | https://support.apple.com/ |
| Edge | Configuración > Ver configuración avanzada > Privacidad y servicios > Cookies | https://support.microsoft.com/ |
La siguiente tabla recoge la clasificación y descripción de las cookies utilizadas en la presente página web para que puedas identificarlas en tu navegador:
| Nombre | Titular | Datos recabados | Finalidad | Duración |
|---|---|---|---|---|
| PHPSESSID | Cookie propia (Clínica Planas) |
Sesiones y preferencias del visitante | Necesaria | Al finalizar la sesión con el navegador |
| VISITOR_INFO1_LIVE | De terceros (Youtube) |
Intenta calcular el ancho de banda del usuario en páginas con vídeos de YouTube integrados. | Técnica | 179 días |
| PREF | De terceros (Youtube) |
Es una cookie que almacena las preferencias de visualización y de búsqueda de los videos de youtube: idioma preferido, filtro safe-search, etc. | Técnica | 2 años |
| __cf_bm | De terceros (Vimeo) |
Análisis de tráfico por motivos de seguridad | Técnica | 1 día |
| TS01057d28 | De terceros (Redsys) |
Realización del pago | Técnica | TS01057d28 |
| f5avr1901846005aaaaaaaaaaaaaaaa_cspm_ | De terceros (Redsys) |
Realización del pago | Técnica | Al finalizar la sesión con el navegador |
| f5_cspm | De terceros (Redsys) |
Realización del pago | Técnica | Al finalizar la sesión con el navegador |
| admincookies | Cookie propia (Clínica Planas) |
Gestionar permisos de cookies. | Técnica | 1 año |
| _hjFirstSeen | De terceros (HotJar) |
Esta cookie se utiliza para determinar si el visitante ha visitado el sitio web con anterioridad o si se trata de un nuevo visitante. | Analítica | 1 día |
| _hjid | De terceros (HotJar) |
Establece un identificador para la sesión. Esto permite a la web obtener datos del comportamiento del visitante con propósitos estadísticos. | Analítica | 1 año |
| _hjIncludedInPageviewSample | De terceros (HotJar) |
Determina si la navegación del usuario debería registrarse en un cierto lugar estadístico. | Analítica | 1 día |
| 1P_JAR | De terceros (Google) |
Utilizada por Google para almacenar información sobre cómo utiliza usted el sitio web , la publcidad y las búsqeudas en Google para ofrecerle una publicidad más personalizada y relevante. | Publicitaria | 1 mes |
| CONSENT | De terceros (Google) |
Utilizada por Google para almacenar las preferencias de publicidad de la red de Google para su uso en la publicidad dirigida. | Publicitaria | 2 años |
| AEC | De terceros (Google) |
Comprueba que las solicitudes que se hacen durante una sesión de navegación proceden del usuario y no de otros sitios | Analítica | 6 mes |
| _hjIncludedInSessionSample | De terceros (Hotjar) |
Registra datos del comportamiento del visitante en la web | Analítica | 1 día |
| _hjSessionUser | De terceros (Hotjar) |
Registra datos del comportamiento del visitante en la web | Analítica | 1 año |
| _ga, _ga_[ID], _gid, _gat_UA-[ID] & _gat_gtag_UA_[ID] | Cookie propia (Google) |
Sesiones de los visitantes. _ga, _ga_[ID] y _gid: Se usan para distinguir a los usuarios. _gat_UA-[ID] & _gat_gtag_UA_[ID]: Se usa para limitar el porcentaje de solicitudes y analizar el tráfico. | Analítica | 2 años - _ga & _ga_[ID]: 2 años. _gid: 1 día. _gat_UA-[ID] & _gat_gtag_UA_[ID]: 1 minuto. Para más información: Política de Cookies de Google |
| player | De terceros (Vimeo) |
Funcionamiento y gestión de los vídeos de vimeo. | Analítica | 1 años |
| vuid | De terceros (Vimeo) |
Funcionamiento y gestión de los vídeos de vimeo. | Analítica | 2 años |
| _fbp | Cookie propia (Facebook) |
Visitas a webs para remarketing | Publicitaria | 90 días |
| YSC | De terceros (Youtube) |
Registra una identificación única para mantener estadísticas de qué vídeos de YouTube ha visto el usuario. | Publicitaria | Al finalizar la sesión con el navegador |
| GPS | De terceros (Youtube) |
Registra una identificación única en dispositivos móviles para permitir el seguimiento según la ubicación geográfica por GPS. | Publicitaria | 1 día |
| IDE | De terceros (Doubleclick) |
Preferencias, enlaces, conversiones e interacciones con anuncios publicitarios. | Publicitaria | 1 año |
| test_cookie | De terceros (Doubleclick) |
Cookie de prueba utilizada por Google DoubleClick para comprobar que se pueden establecer cookies de publicidad. | Publicitaria | 1 minuto |
| TDID | De terceros (The Trade Desk) |
Esta cookie lleva información sobre la forma en que el usuario final utiliza el sitio web y cualquier publicidad que el usuario final pueda haber visto antes de visitar dicho sitio web. | Publicitaria | 1 año |
| _gcl_au | Cookie propia (Google) |
Visitas a webs para remarketing | Publicitaria | 3 meses |